The following is a guest article from Doc Martyn. His opinions and advice are entirely his own. His contact information can be found at the end of the article.
1. Mr. Mike’s love affair with cigarettes began 45yr ago, when he was 18 years old. Since then, he has smoked 20 cigarettes a day. He does not have an addictive personality. He does not drink alcohol. He does not use drugs. He does not gamble. “Smoking is my only vice and I enjoy it.” He says.
On December 9th 2023 he suffered central chest pain; ‘Like a weight on my chest’ and pain in his left arm. His local doctor sent him to the Bangkok Hospital Pattaya (BHP) to manage his ‘heart attack’, which they did. Mr Mike did not have a myocardial infarct; his pain was severe angina pectoris only.
After 3 hours, once stabilised he was discharged home with an appointment on 18th December for a coronary angiography. His care at the BHP was free of charge, but his angiography would cost THB 400,000. If stenting was required the charge would be considerably higher.
2. He came to see me on December 13th. He presented as a robust man, 183cm tall weighing 100kg, who was unstable on his legs. He suffered ataxia due to Wallenberg’s syndrome, also known as Lateral Medullary syndrome.
Ostensibly, in 2021 whilst playing pool in a bar his legs became weak. He went home to rest. In the morning he was unable to move his legs. He could not stand. He was hospitalised at BHP for 3 days, where the diagnosis of Wallenberg’s syndrome was made.
3. Wallenberg’s syndrome is caused by a stroke in the brain stem from reduced blood flow in the Posterior Inferior Cerebellar Artery (PICA). Mr Mike’s stroke was not severe. He rehabilitated well. The BHP discharged him on Apolets 75mg (Clopidogrel; an antiplatelet medication or ‘blood thinner’) and Chlovas 40mg (a statin). Both treatments were appropriate. But the doctors did not advise him to stop smoking, smoking being one of the causes of Wallenberg’s syndrome.
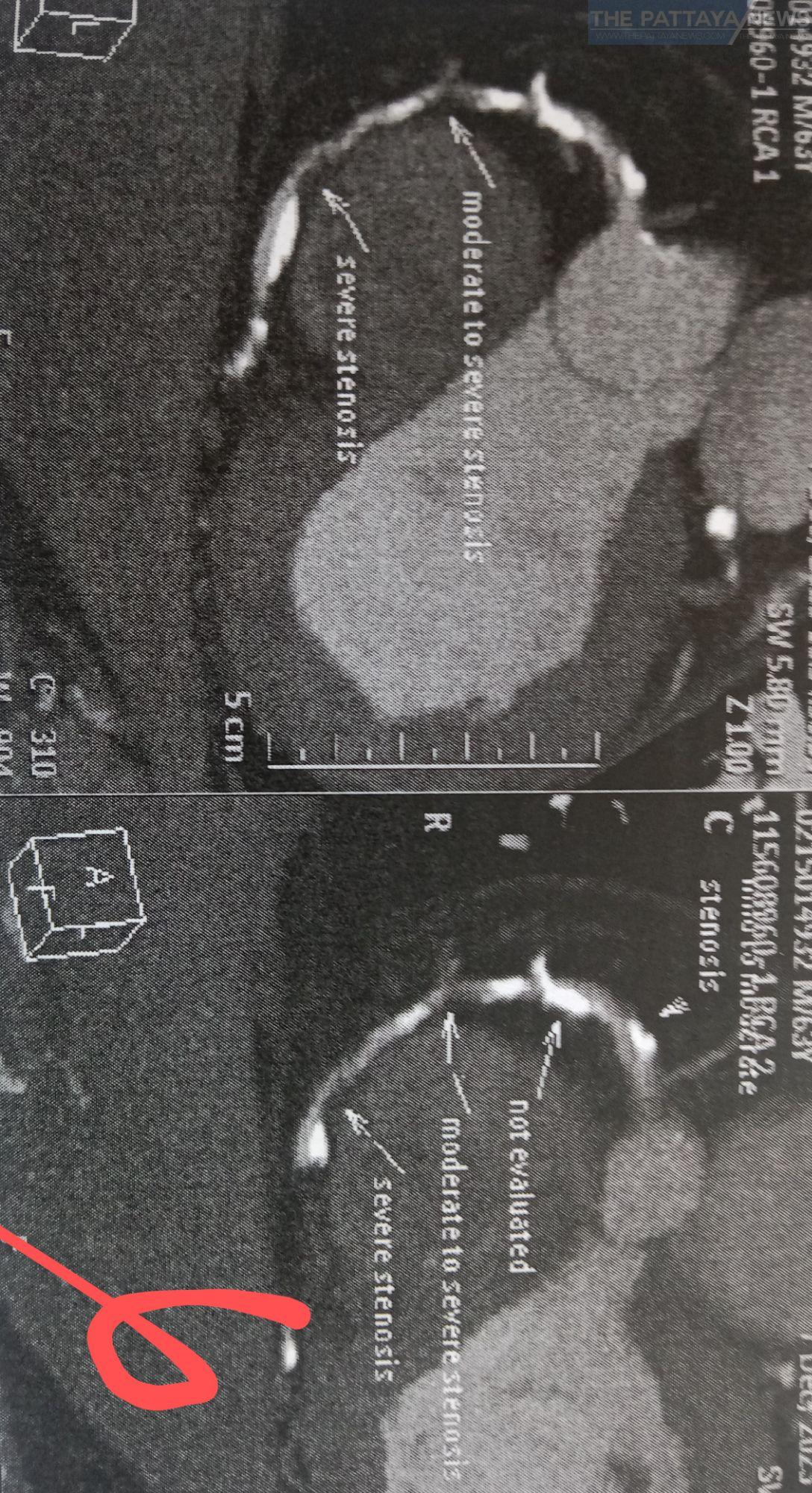
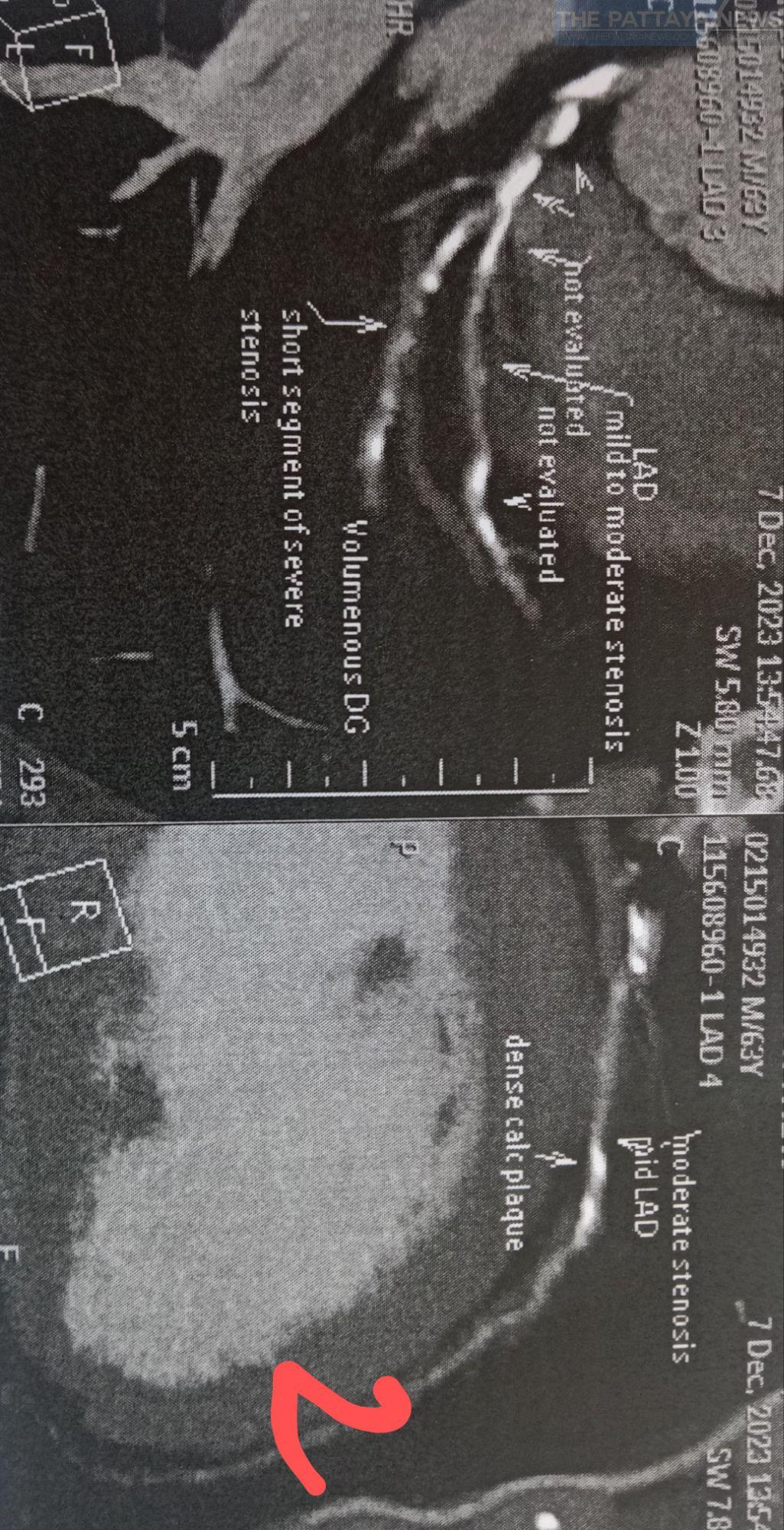
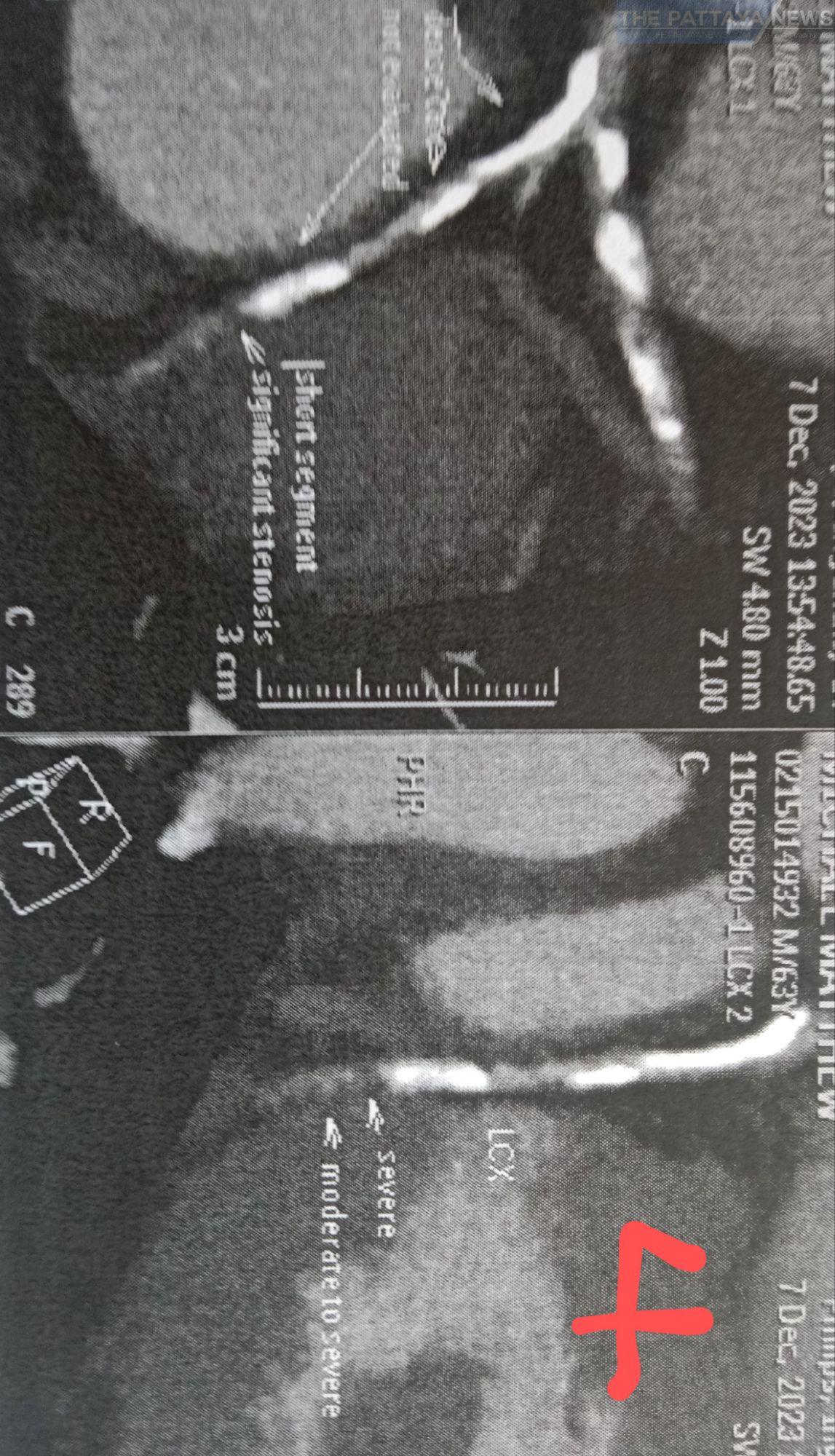
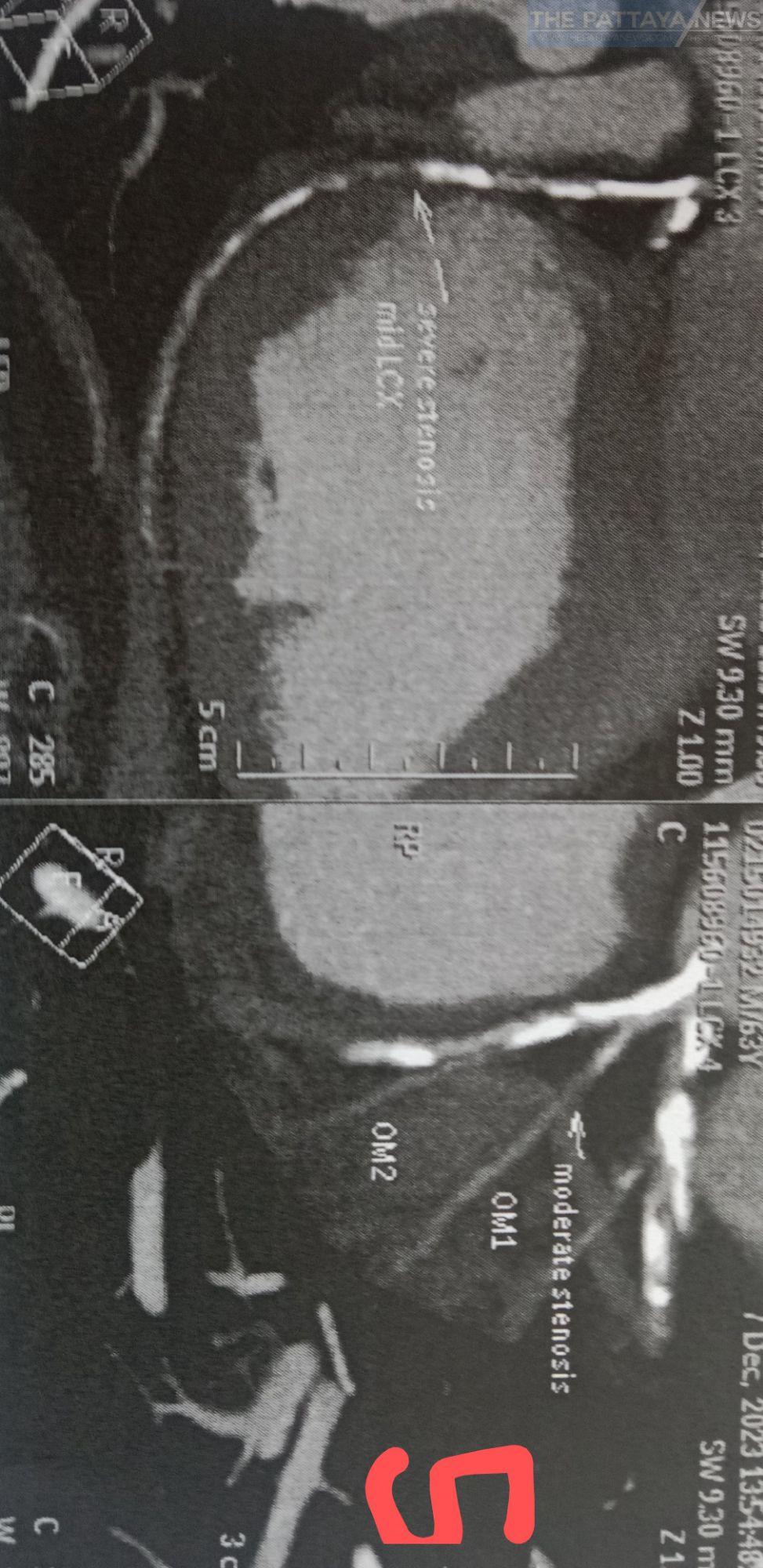
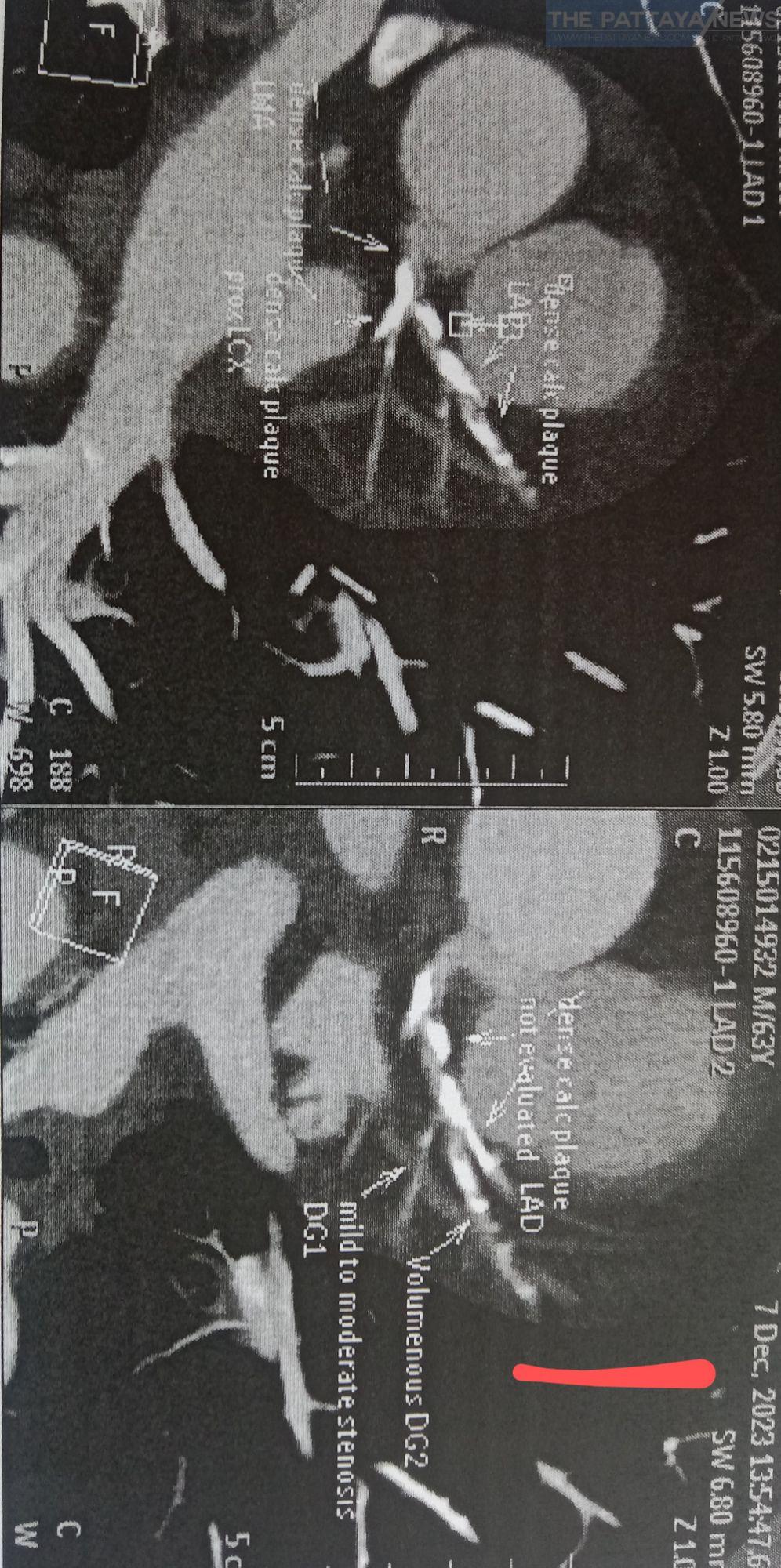
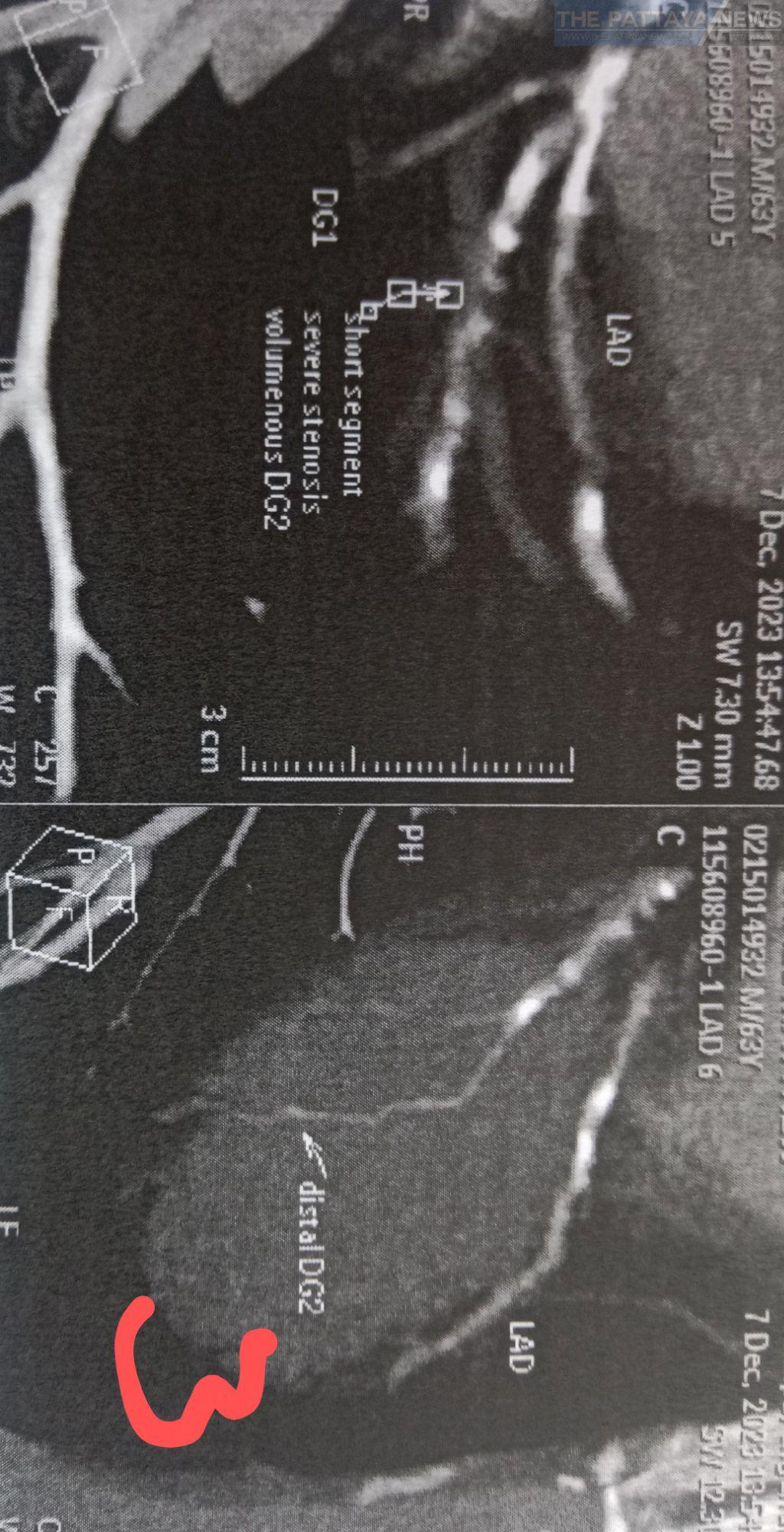
4. During his consultation I reviewed his Coronary Calcium CT scan performed on December 9th by the BHP. He had extensive and significant calcium deposits throughout his coronary arteries, see photos 1-6.
His calcium Score was 1,775.57, which puts him in the 97th percentile. This means that 97% of patients in his age group would have less calcium in their coronary arteries and 3% would have more than him. This is serious. If left untreated, Mr Mike was at risk of sudden death.
5. Mr Mike’s physical examination was unusual:
Left arm: BP 106/77, pulse 84 SR (Sinus Rhythm; the medical term for normal rhythm), heart sounds were normal but he had a faint bruit, murmur, in his upper left chest below his collar bone.
For a man of his stature, I expected his BP to be higher. I questioned him about his BP. He reassured me that his normal BP was much higher. I measured his BP in his right arm. The reading was 137/91.
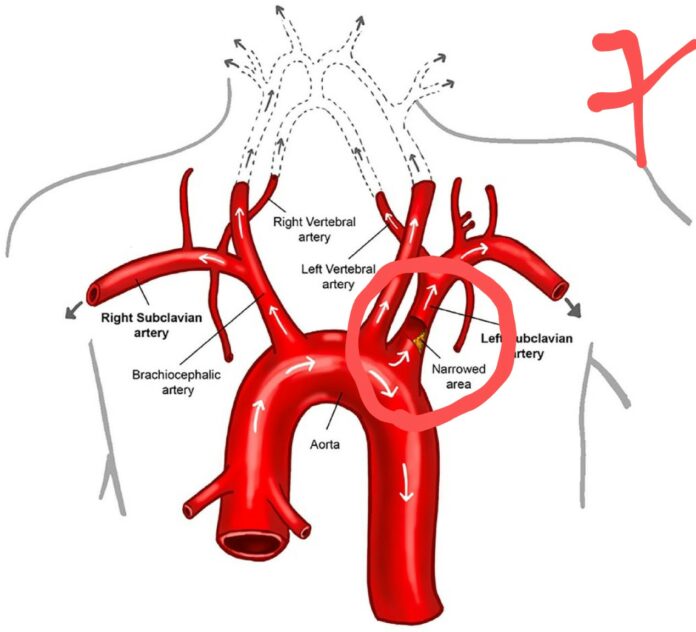
Mr Mike had atherosclerotic stenosis at the origin of his left brachial artery which was causing the murmur and restricting the blood flow into his left arm, causing the low BP.
Clearly, it was this stenosis which caused his Wallenberg’s syndrome, a clot from the stenosis travelled up his PICA causing the stroke. see photo 7 the PICA branches from the Vertebral artery.
So, in addition to his Coronary Artery Disease (CAD), Mr Mike has Peripheral Vascular Disease (PVD). He is seriously ill and his illness is directly related to his 45-year attachment to cigarettes.
6. It was imperative to reduce Mr Mark’s atherosclerotic burden.
I gave him the following advice:
Stop smoking.
Cancel the scheduled angiogram and stenting of his heart.
Double his statin dose to Atorvastatin 40mg twice/day.
Start Isosorbide mononitrate 10mg twice/day.
The rationale behind these instructions:
Stop smoking: Empiric medical evidence indicates that smoking cigarettes causes atherosclerosis.
Cancel the angiogram: In addition to the calcium deposits in the walls of his heart arteries, the CT identified significant coronary atherosclerosis.
There are two main arteries in the human heart; the left and the right coronary arteries. These arteries do not connect. If, however, one or both arteries become compromised, over time the two arteries grow and join.