Medical Bytes No 97: “Legless in Thailand”
Originally Published 30/9/23
Editor’s Note: Some pictures in this opinion editorial could disturb sensitive viewers. Viewer discretion is advised. All pictures are at the end for those who may only want to read the story.
1. Alex messaged me on May 9, 2023.
His story: ‘On April 13th, 2023, I took a tumble on the golf course and landed on my left knee and shoulder. I attended the local clinic to get antibiotics for the cuts and scratches on my knee. I noticed that I had 3 quite strange looking, non-tender, red marks, under the skin, above my left ankle. After a week, the skin turned black and became painful, photos 1 and 2. I attended the local hospital……..I was told to take broad spectrum antibiotics and attend the local health clinic daily for dressing. The pain increased. It felt like boiling water was being poured over the skin, photos 3 & 4 are the wounds after 2 weeks. Can you have a look and let me know your thoughts.’
2. We talked later that day. I told him that he needed hospital care for identification of the bacteria in his wounds followed by appropriate I/V, intravenous, antibiotics.
Alex was admitted to hospital on May 10. He was given the I/V antibiotic, Clindamycin.
I advised him that he would probably require additional antibiotics.
On May 12, he sent me the following message: ‘The doctor told me yesterday that they wanted to send me to Udon Thani for an operation to cut away the infected meat etc. Said I would lose skin but keep foot…Feeling slightly less pain today, and more mobile today so I convinced her to leave another 2 days before final decision… You have any recommendations?’
I called him in the early afternoon. We talked at length. I told him that the mainstay of treatment was I/V antibiotics to kill the bacteria that was causing the ulcerations of his leg. Unless the I/V treatment failed, I advised him against tissue removal. If he did consent to tissue removal he must request a split-skin graft to assist the repair of the open wound(s).
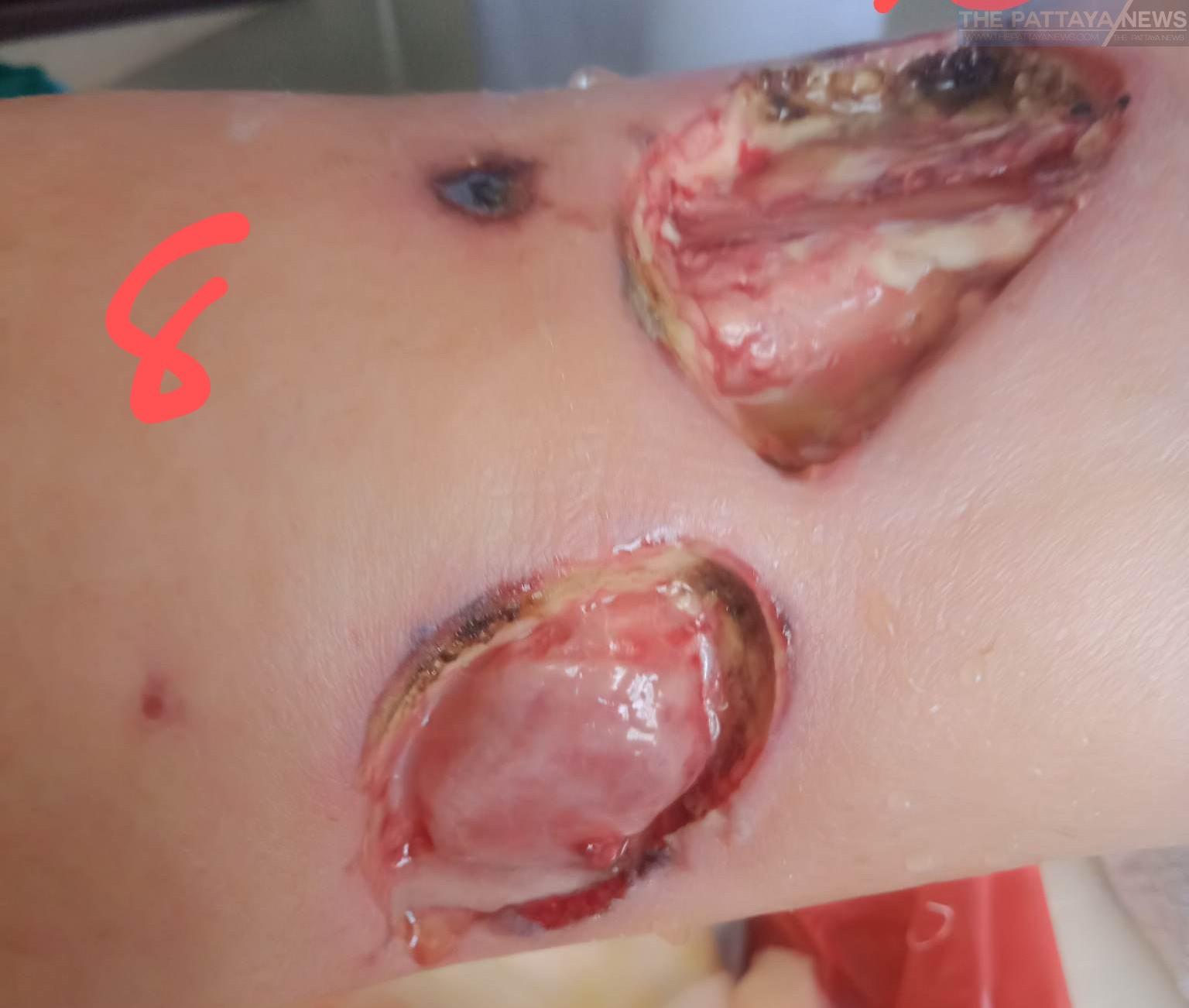
3. On May 20, Alex sent me pictures of the tissue removed from his left leg, see photos 5, 6, 7, 8, with the message: ‘Hi Doc I was a wee bit reluctant to send you these as I know you will be angry. They basically conned me into letting them do this. You have any advice on best way to regenerate the flesh’. I advised ‘a split skin graft’. Alex replied: ‘Cheers, the surgeon told me he had only removed dead or badly infected materials, nearly fell over the first time they changed the dressings…..Doctor says all infection cleared up so no need for oral antibiotics.’
We had no further contact until September 4th, 2023 when I saw his posts on Facebook about his amputation.
4. Ostensibly, following his discharge from hospital the infection returned (as did his horrors!) The flesh of his leg continued to be eaten away by infection and the surgeon continued to remove tissue from his leg. Eventually, the surgeon removed his leg with a below knee amputation. Alex was sent home the next day!
Within 3 days the infection appeared in the stump. He was admitted to the ‘Sepsis Zone’ of the public hospital. He lay amongst the septic sick and the dying Thais, in their faeces soiled sheets. Many of the patients had no family to attend to their needs. The night care was rudimentary. And the few night nurses available remained busy on their mobiles.
Eventually, a private room became available, in which Alex found a modicum of sanctuary before the final insult. He required a mid-thigh amputation to remove his infected stump.
He is now rehabilitating at home.
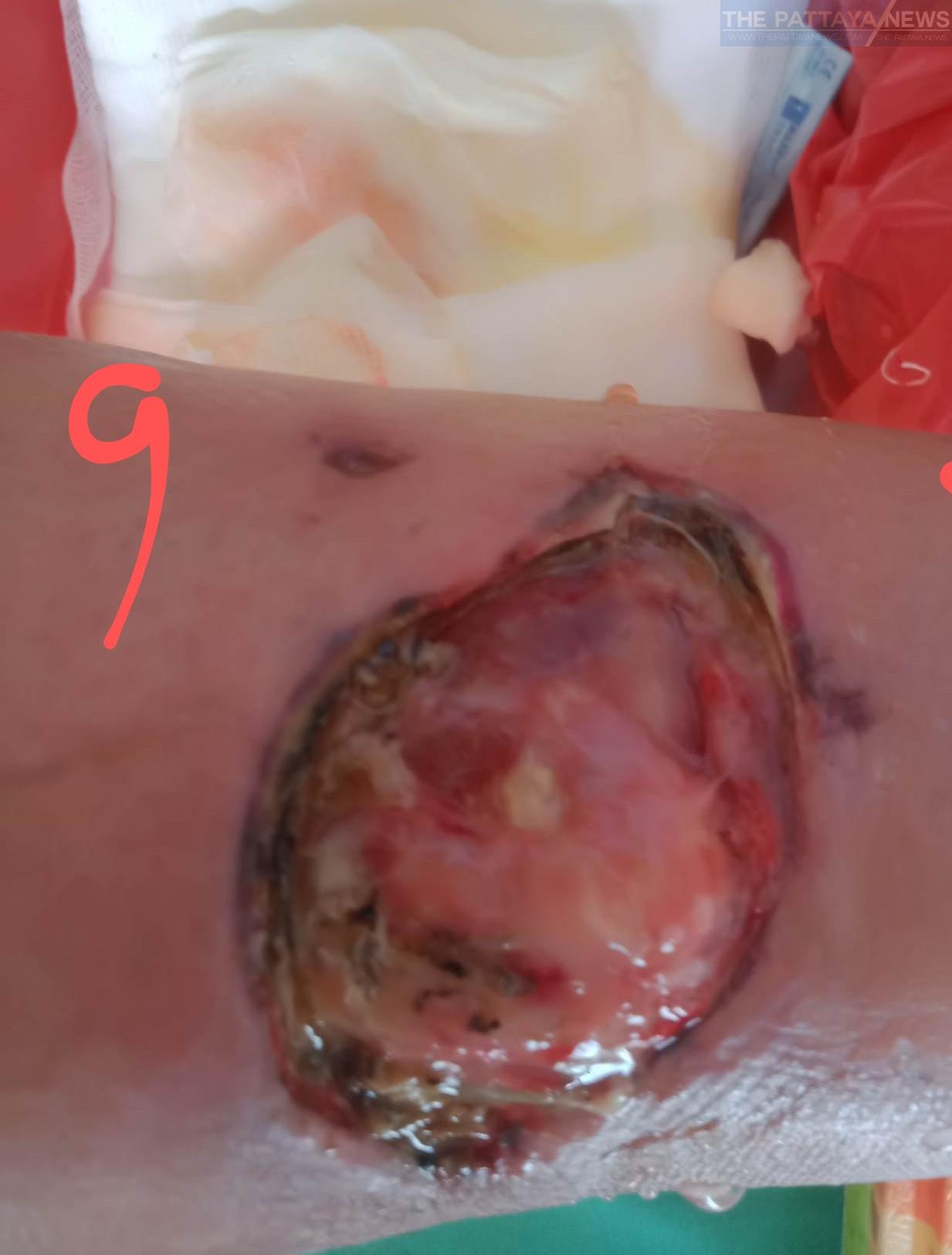
5. Alex’s story of painless red marks around the ankle that turned black in the middle, becoming tender then very painful, is typical of Necrotising Fasciitis, aka flesh eating disease, see example photo 9, not Alex. When Necrotising Fasciitis spreads it rapidly becomes a fatal disease, see photo 10, not Alex.
There are four types of Necrotising Fasciitis:
Type 1: Polymicrobial, more than one, bacterium involved.
Type 11: Group A haemolytic streptococcus +/- Staphylococcus, including Golden Staph, aka Methicillin Resistant Staphylococcus Aureus, MRSA.
Type 111: Gangrene
Type 1V: Marine organisms and fungus.
Necrotising Fasciitis is a very serious illness with a 20-35% mortality rate.
In 2018, the incidence of Necrotising Fasciitis in Thailand was 32.46 per 100,000 of population/year. The incidence in America is 0.4 per 100,000 of population/year and in Europe 1 per 100,000 of population/year.
6. The management of Necrotising Fasciitis; hospital admission and proper wound care and handwashing. The treatment includes swabbing the wound, to culture the infection, enabling identification of the bacteria involved. Then treat with the appropriate I/V antibiotics. If the illness does not respond, early surgical intervention is essential.
7. Alex had Type 1 Necrotising Fasciitis. His wounds remained local.
So, why did he lose his leg?
-Type 1 Necrotising Fasciitis was not diagnosed early.
-Early admission to hospital was required, but even after his lesions became painful, he was managed by his local clinic and in the out-patients.
-Once admitted, his wounds were not swabbed, in fact throughout his ordeal no swabs were taken at any time. Thus, the bacteria were never identified and the correct antibiotics were not given.
-Alex was only treated with Clindamycin.
-Alex would have responded to the correct I/V antibiotics if they had been prescribed, obviating the need for amputation.
-In Type 1 Necrotising Fasciitis, an adequate trial of focussed antibiotics should clear the infection. Surgical excision is only indicated if the antibiotic therapy fails.
-Despite the surgeon’s reassurance, he failed to remove all the infected tissue, note the black dots of infection in photos 5, 6, 7 and 8.
Post amputation, Alex complained to me about the eleven Thai doctors who managed him throughout his ordeal. “They didn’t appear to know what they were doing and they would not discuss my case with me”.
The cost to Alex of this poor management; his left leg and GBP 25,000.
8. International medical boards consider the Thai medical school training to be inadequate. A Thai qualified doctor cannot work in the West without additional training and qualification(s).
Necrotising Fasciitis is a terrible illness, to which many succumb. If you have a red lesion that becomes black and painful anywhere on your body, do not go to your local Thai clinic. Do not rely on the homegrown Thai doctors and their manifestly inadequate medical training. Visit a private hospital that has overseas trained Thai doctors although some chains have homegrown doctors.
Be careful, do not become “Legless in Thailand”.
Contact him at his Facebook on the above link.