Originally Published 4th June 2023.
- Nick, a 42-year-old Farang domiciled in Thailand, contacted me on 21st May 2023, the day after he was released from the hospital.
Apparently, Nick had been experiencing intermittent right lower quadrant abdominal pain and an ache in his left lower chest that radiated into his back and epigastrium. He had been generally unwell for two weeks.
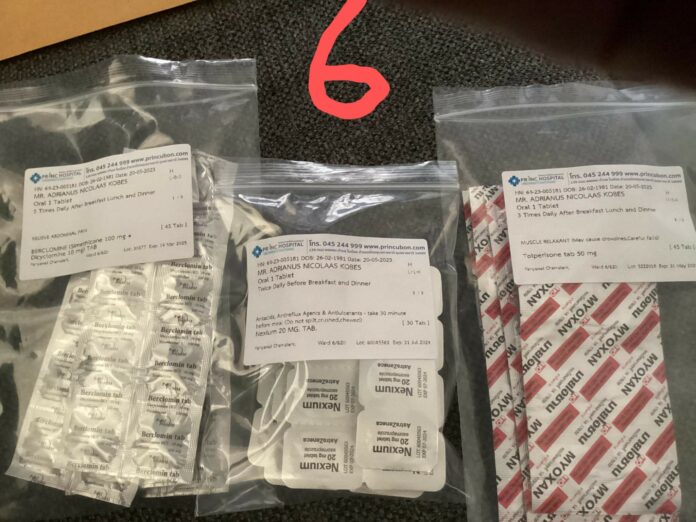
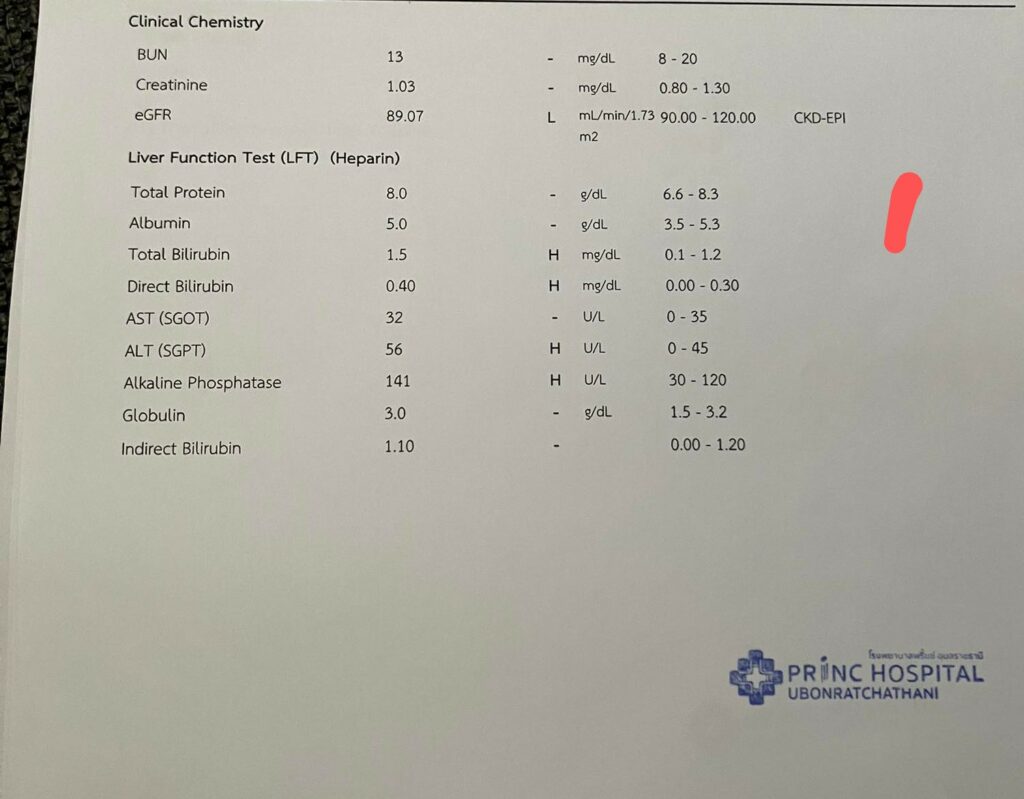
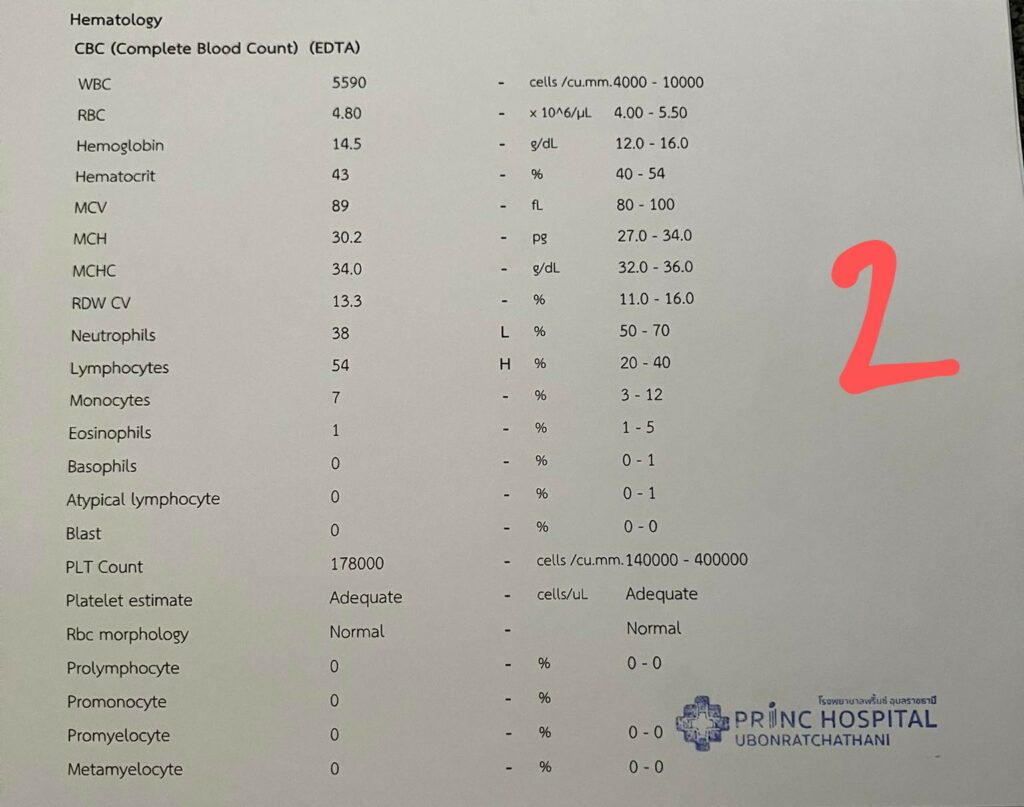
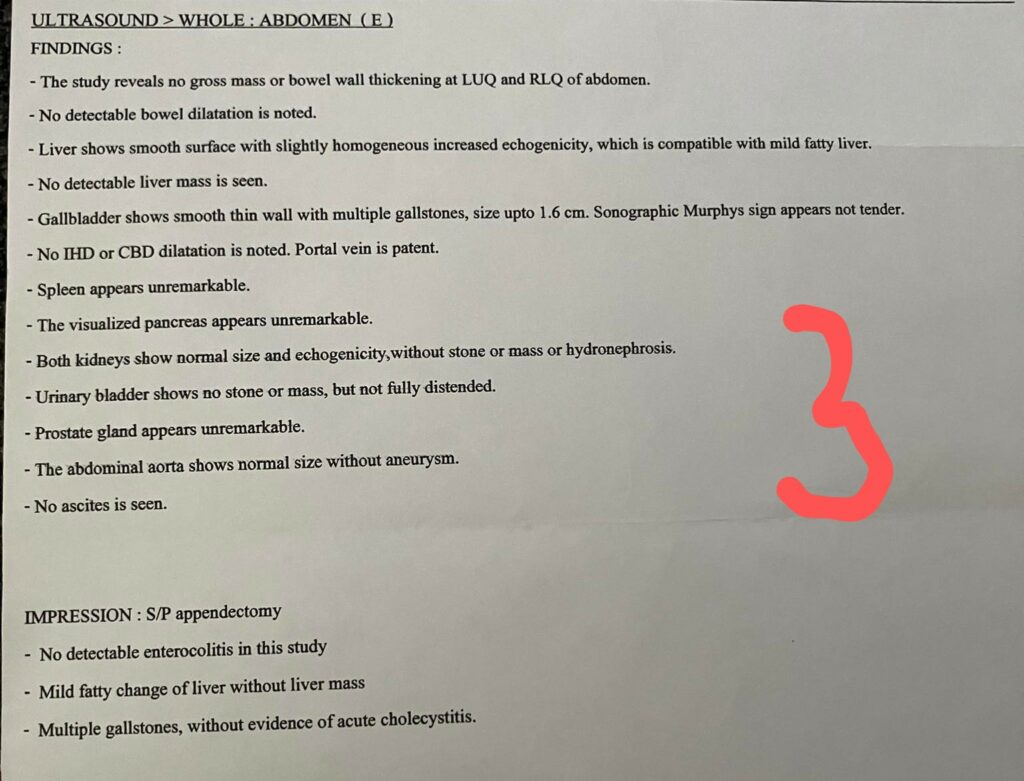
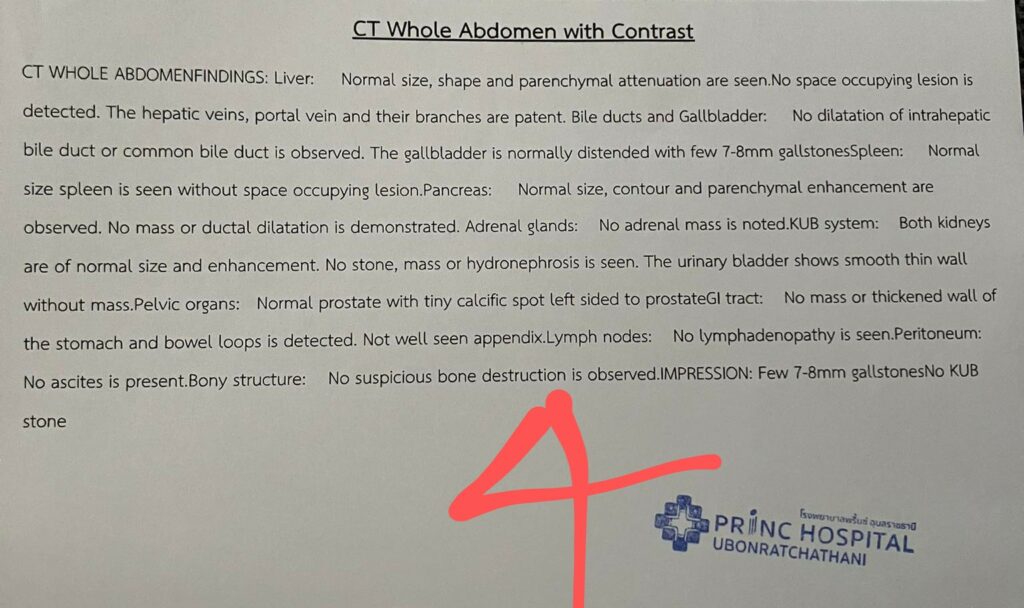
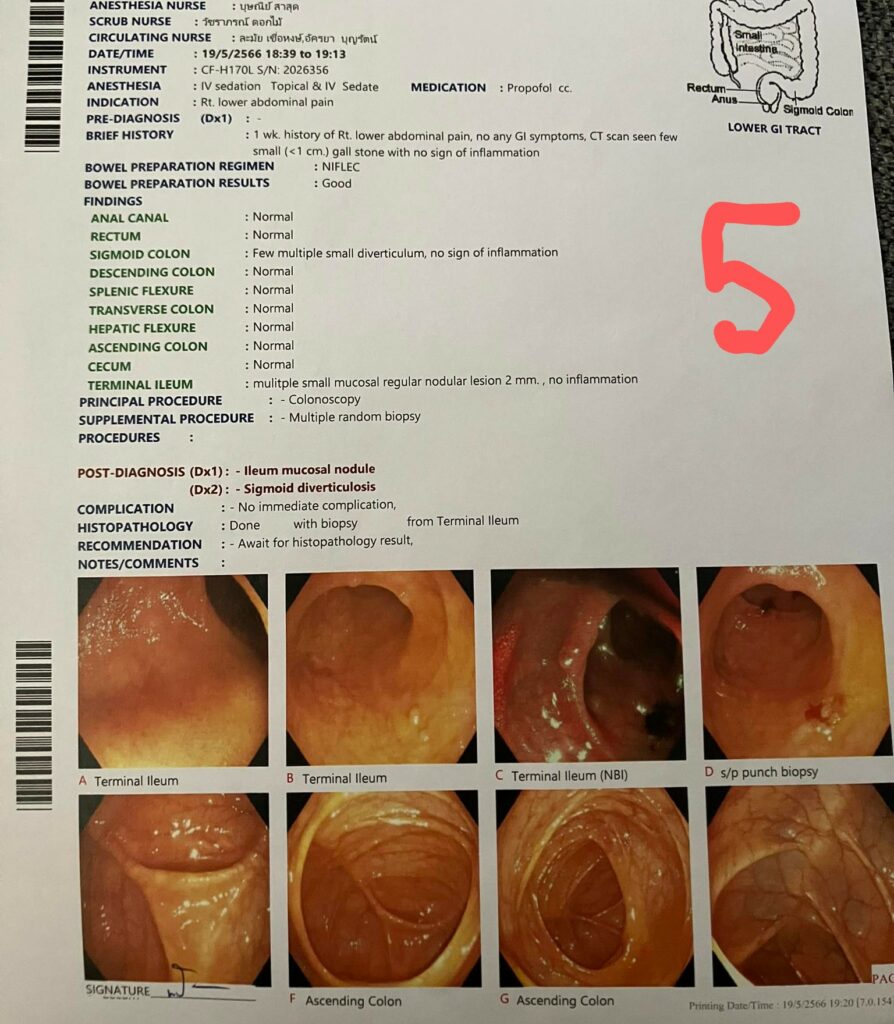
He was admitted to the hospital and processed by a gastroenterologist who ordered pathology, see photos 1 and 2, abdominal ultrasound, see photo 3, and a CT of Nick’s abdomen, see photo 4. He also underwent a colonoscopy, see photo 5.
- Pathology results from 1 & 2 indicate that Nick had raised bilirubin levels and his liver was damaged (raised ALT and Alkaline phosphatase). In addition, his white cell count was abnormal, suggesting inflammation and/or infection.
The ultrasound showed multiple gallstones, the CT abdomen confirmed multiple, 7-8mm, gallstones. The colonoscopy demonstrated mild colonic diverticulosis.
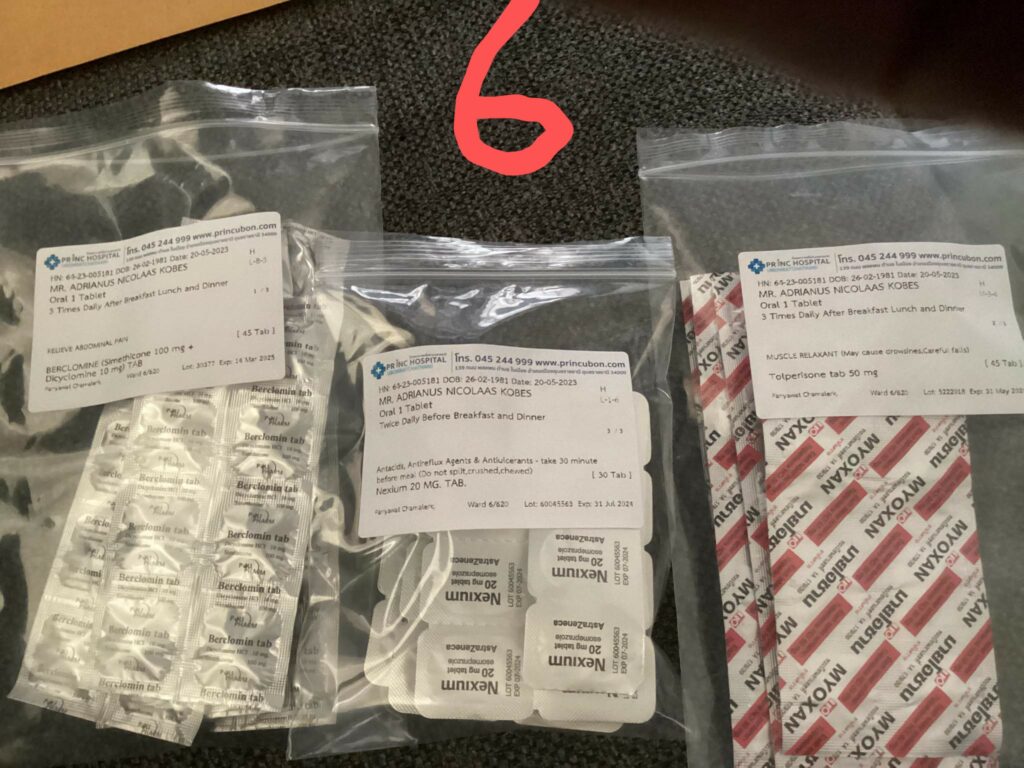
- I asked Nick to send me a photo of his prescribed medication, see photo 6, which consisted of Dicyclomine; for stomach spasms and irritable bowel syndrome, Nexium; to reduce stomach acid, and Myoxan, a smooth muscle anti-spasmodic.
Nick left the hospital without a diagnosis; he was unsettled and disappointed. And so he should have been; the drugs prescribed were to reduce the acid level in his stomach and any associated smooth muscle spasm.
This management decision, made by the specialist, was “a bad call”.
- I talked with Nick on 21st May. I explained the seriousness of his condition. His blood tests indicated that he was suffering significant consequences from his gallstones. The obstruction produced by his gallstones was causing his lower chest, epigastric and back pain. I advised Nick to have his gallbladder removed immediately.
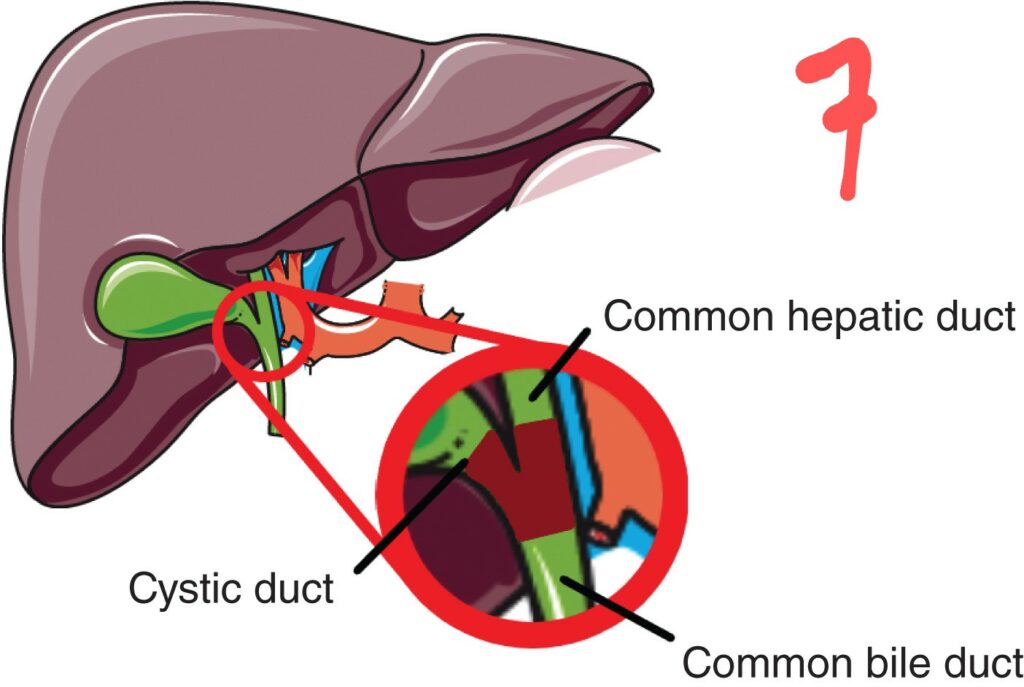
- The gallbladder, known medically as the Cholecyst, is a hollow pear-shaped organ that drains into the cystic duct, thence the common bile duct, and finally into the small bowel.
Following the ingestion of fat, the gallbladder contracts to push its contents, bile salts, into the cystic duct and beyond. (Bile salts emulsify the fat and facilitate its digestion).
Large and small gallstones are usually not problematic; small stones pass freely through the ducts; large stones are too big to enter the duct. They remain in the gallbladder.
In younger people, the cystic duct, see photo 7, is about 6mm in diameter. 7-8mm gallstones are potentially dangerous: When the gallbladder contracts, 7-8mm stone(s) may be pushed into the cystic duct, causing obstruction of the duct. This results in inflammation of the gallbladder; Cholecystitis.
A stone that obstructs the common bile duct causes ascending Cholangitis, which damages the liver.
A stone obstructing the lower common bile duct will impede the outflow of the pancreas, causing Pancreatitis.
- Nick’s appointment with the surgeon was in the afternoon of May 23rd. As I expected, the surgeon was reluctant to remove his gall bladder. Nick called me and put the surgeon on speakerphone. The surgeon’s immediate reaction: ‘Lower abdominal pain is not caused by gallstones. I explained that Nick was suffering chronic gallbladder outflow obstruction, which caused his elevated bilirubin levels, his liver damage, and his pancreatic pain. The surgeon remained speculative and resistant. To investigate the cause of Nick’s lower abdominal pain, I suggested that; following the laparoscopic removal of Nick’s gallbladder, the surgeon could turn the scope towards his lower abdomen to visualize Nick’s right lower quadrant. The surgeon conceded that that was a good idea.
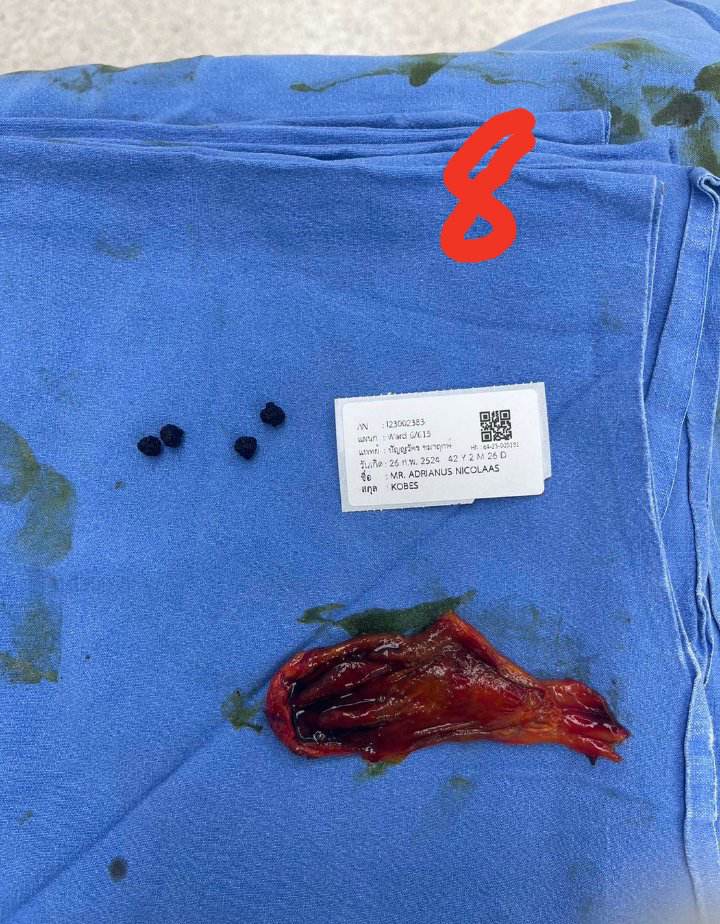
- Nick was operated on the following morning at 06:00hrs, May 24th.
His gallbladder and the contained stones were removed successfully, see photo 8. The cause of Nick’s lower abdominal pain; post appendicectomy adhesions. These were released, see videos.
Nick’s recovery was rapid. He was discharged from the hospital on May 26th, when he was feeling, and I quote: “100 times better”.
- The pathology report on Nick’s gallbladder confirmed that he was suffering from chronic cholecystitis. The blood sample taken a week after his operation indicated that Nick’s liver was in recovery and that his pancreas was normal.
The prompt attention to Nick’s plight relieved him from years of chronic pain and ill health.
In medical parlance, this was “a good call”.
The preceding is a regular guest piece by Doc Martyn. His statements and opinions are his own.